Mechanism of Dysfunction
The main predisposing factor for the development of plantar fasciitis is the impaired foot mechanics caused by a compromised of the arches (see Flat foot page for detailed information), causing the foot to lose its intrinsic shock absorption support, increasing the horizontal distance between the heel and the toes and eventually overstretching and damaging the fascia. Due to the compromised of the transverse arch, the middle cuneiform bone misaligned down and causes a direct irritation of the fascia.
Assessment Protocol
The entire lower extremity biomechanical chain must be evaluated as part of the foot/bunion analyses as per the neurological and mechanical influences of the spine, hip, and knee.
Clinical assessment to identify the key joint dysfunctions of the Ankle/Foot that have contributed to a compromised arch. Soft tissue analysis to pinpoint the level of irritation.
X-ray analysis
Anterior – Posterior (AP) X-ray ankle view is essential for proper diagnosing the master joint of the ankle (Tibia-Talus) as the origin of poor arch mechanics starts from a dysfunctional ankle joint leading to hypermobility compensations that causes the appearance of the plantar fasciitis
Lateral Xray view is important to check the degree of the total arch compromised, specially the medial arch as per the direct influence it has with this deformity.
MRI
Foot MRI is essential for:
Locate the exact injury point; Allows the treatment to be more specific during the application of the treatment modalities
Identify the extent of tissue damage and the presence of scar tissue; Provides valuable information in regard to prognosis and the application of friction soft tissue modalities to aid on scar tissue removal.
Rule out any other condition that might mimic plantar fasciitis; There are rare disorders that may create similar patterns of dysfunction, is advisable to rule out these conditions prior to the start of the treatment.
Treatment protocol
Due to the influences the foot arches have in the development of plantar fasciitis, arch rehabilitation must be incorporated as part of the overall treatment.
The treatment care should aim to restore the foot/ankle alignment and the soft tissue muscles and fascia layer.
Foot Arch treatment: Specific adjustments of key bones of the ankle and foot (Talus, Navicular, Calcaneus and Cuboid) followed by a rehabilitation regime to strengthen the entire soft tissue arch support of the foot. In addition, application of tape and corrective orthotics may be needed as part of the early rehab program.
Plantar fascia treatment
Adjustment of the middle cuneiform as per the direct influence it has with the plantar fascia.
Application of Low-level Laser and PEMF to aid on the cellular level of heling as well as improving the microcirculation for the area.
Friction soft tissue therapy helps to reduce dysfunctional scar tissue
Specific stretches and strengthening to improve the resilient of the soft tissue support
Functional tape might be used to decrease the horizontal sheering forces at the fascia
Specific selected essential oil application to enhance healing
Depending on the level of arch compromised and chronicity of the bunion a minimum of 6 weeks up to 12 weeks of treatment care may be necessary to resolve this deformity.
Related Conditions
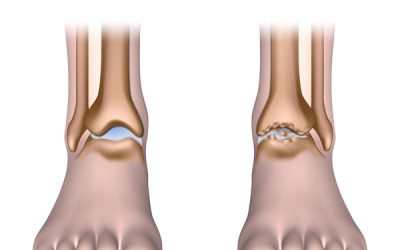
Ankle arthritis
Mechanism...
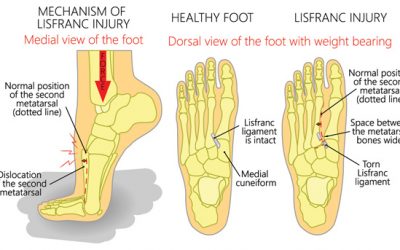
Lisfranc Sprain
Mechanism...
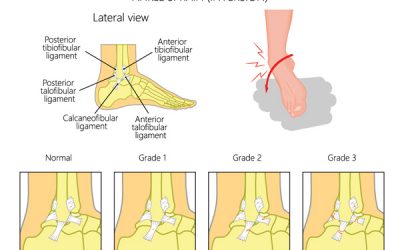
Inversion Ankle Sprain
Patients report of...