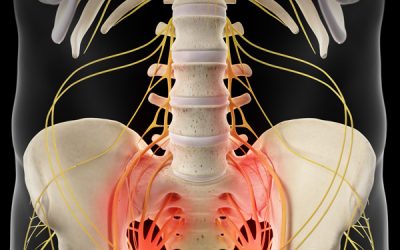
The alignment of the pelvic girdle and to a lesser extent the Hip joint are key structures involved and responsible for maintaining the health and resilient of the soft tissue support. All the hip muscles attached at the pelvis and the tendons are used as powerful leverages to aid on the required movement. When the pelvis misaligned, certain muscles groups becomes shorten and the opposing muscles becomes overstretched creating the ideal scenario for the development of the different types of tendinopathies.
Pelvic misalignments and the associated tendon/bursa and muscle injury
Pubic joint misalignment – Adductor Tendinitis/Strain,

Internal or External pelvic misalignment – Snapping Hip Syndromes, Iliotibial band (ITB) syndromes, Trochanteric Bursitis.
 Trochanteric Bursitis
Trochanteric Bursitis
Posterior or Anterior pelvic misalignment – Hamstrings Tendinitis, Rectus Femurs Tendinitis/Sprain, Iliopsoas Tendinitis/Sprain, Psoas bursitis, Iliopectineal bursitis
- Hamstring-tendinitis
- Rectus-femoris-tendinits
- Iliopsoas-muscles
Mechanism of injury
One the lumbar/pelvic dysfunction is installed; the location of the injury will be dependent on the mechanism of the trauma. For instance, activities that involve flexion and extension hip movements predisposed to a particular location of injury different from the abduction and adduction movements.
Assessment
Clinical evaluation of the pelvic girdle and hip alignment and specific orthopaedic tests to pinpoint the location of the injured muscle/tendon
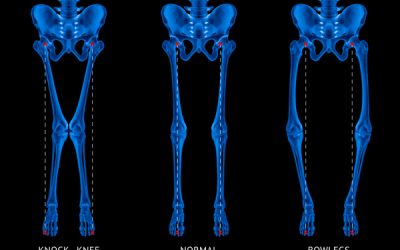
X-ray
Anterior – Posterior (AP) X-ray Pelvic/Hip views are essential to analyse the level and direction of the different patterns of misalignments
MRI
Locate the exact injury point; Allows the treatment to be more specific during the application of the treatment modalities, in addition, aids to identify the type of tendinopathy (tendinitis or tendinosis) and the corresponding appropriate treatment care.
Identify the extent of tissue damage and the presence of scar tissue; Provides valuable information regarding prognosis and the application of friction soft tissue modalities to aid on scar tissue removal.
Treatment Protocol
Specific Pelvic and hip adjustments followed by a rehabilitation regime to strengthen the entire soft tissue support.
Application of Low-level Laser and PEMF to aid on the cellular level of heling as well as improving the microcirculation for the area.
Friction soft tissue therapy helps to reduce dysfunctional scar tissue
Dry needling may be used to improve local blood flow and to reduce the deep muscle tension.
Specific selected essential oil application to enhance healing
Depending on level of misalignment and chronicity a minimum of 6 weeks up to 12 weeks of treatment care may be necessary to resolve this deformity.