The alignment of the knee and pelvic girdle and to a lesser extend the Hip joint are key structures involved and responsible for maintaining the health and resilient of the soft tissue support. All the knee muscles have their origin attachment on pelvis and inserted point on the knee. Their corresponding tendons are used as powerful leverages to aid on the required movement. Therefore, when the knee and pelvis are misaligned, certain muscles groups becomes shorten and the opposing muscles becomes overstretched creating the ideal scenario for the development of the different types of tendinopathies and muscles injuries.
Knee tendinopathies can be extremely painful as per the concentration of nerve receptors accumulated on the tendon. Generally, patients report a localised sharp pain in the tendon involved, causing everyday tasks such ass walking and climbing stairs quite difficult.
Knee and pelvic misalignments and the associated tendon/bursa and muscle injury
Posterior/Anterior pelvic misalignment and posterior Tibia dysfunction are commonly associated with Patellar tendon Tendinitis or tendinosis (Jumper’s Knees) , Pre, supra, infra – Patellar bursitis, Biceps femoral tendinitis, Hamstrings injuries and Baker’s cysts.
- Hamstring-tendinitis
- Knee-bursitis
- Baker-cysts
- Patella-tendinitis-
- Biceps-tendinitis
Internal or External pelvic misalignment and Rotational Femur disfunction are commonly associated with Pes Anserinus Tendinitis/Bursitis and, Iliotibial band tendinitis/Bursitis (Runners Knee)
- iliotibial-band-tendinitis-and-bursitis
- Pes-anserine-bursitis-and-tendinits
Mechanism of injury
Once the pelvic/knee dysfunction is installed; the location of the injury will be dependent on the mechanism of the trauma. For instance, activities that involves flexion and extension hip and knee movements predisposed to a location of injury different from the abduction and adduction movements.
Assessment
Clinical evaluation of the pelvic girdle and knee alignment and specific orthopaedic tests to pinpoint the location of the injured muscle/tendon
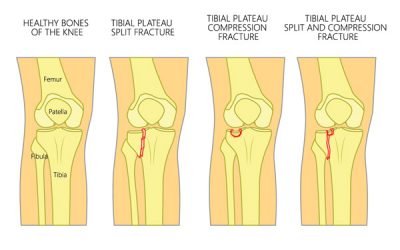
X-ray
Anterior – posterior (AP) and Lateral Knee views are essential imaging to check the different patterns of knee misalignments
MRI
Locate the exact injury point; Allows the treatment to be more specific during the application of the treatment modalities, in addition aids to identify the type of tendinopathy (tendinitis or tendinosis) and the corresponding appropriate treatment care.
Identify the extent of tissue damage and the presence of scar tissue; Provides valuable information regarding prognosis and the application of friction soft tissue modalities to aid on scar tissue removal.
Treatment Protocol
Specific Pelvic and Knee adjustments followed by a rehabilitation regime to strengthen the entire soft tissue support.
Application of Low-level Laser and PEMF to aid on the cellular level of heling as well as improving the microcirculation for the area.
Friction soft tissue therapy helps to reduce dysfunctional scar tissue
Dry needling may be used to improve local blood flow and to reduce the deep muscle tension.
Specific selected essential oil application to enhance healing
Depending on level of misalignment and chronicity a minimum of 6 weeks up to 12 weeks of treatment care may be necessary to resolve this deformity.