Mechanism of Dysfunction
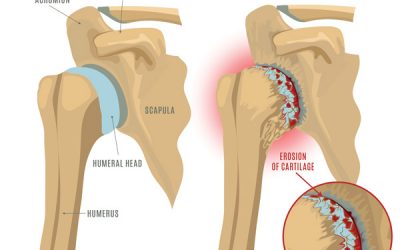
The predisposing factors for the development of this condition began with a misalignment dysfunction at the shoulder complex, which overtime causes the soft tissue ligamentous, muscle and cartilage to become overloaded and compromised allowing the biomechanical stress to gradually reach the level of the bone and resulting in the development of fractures and dislocations.
Types of shoulder fractures and dislocations
Clavicle Fractures, Scapula fractures, Proximal Humerus Fractures.
- clavicle-fracture
- Proximal-Humerus-fracture
Anterior Shoulder dislocation
Posterior shoulder dislocation

shoulder-anterior-and-posterior-dislocation
AC separation

AC-separation
Is important to note that for the bone to become dislocated and injured, the previous defence mechanisms have to have failed to allow the biomechanical stress to damage the bone, therefore, the treatment care must aim to restore the health of the entire shoulder protective structures.
Assessment Protocol
The entire upper extremity biomechanical chain must be evaluated as part of the shoulder analyses as per the neurological and mechanical influences of the spine, elbow, and hand
Clinical assessment to identify the potential areas of the fractures, identify the key joint dysfunctions of the shoulder that have contributed to this condition. Soft tissue analysis to pinpoint the level of irritation in all tissue layers. Check the level of vascularity.
X-ray analysis
Anterior – Posterior (AP), AP internally/externally rotated shoulder and Scapulothoracic views are essential to analyse the level and direction of the different patterns of misalignments and the degree and location of the fracture sites and the exact direction of the shoulder dislocation
MRI
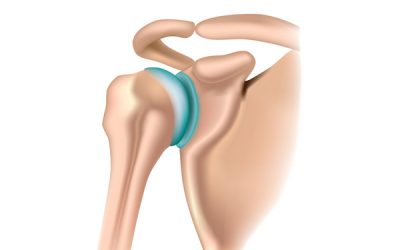
Shoulder MRI is essential for visualizing the extent of injury on the muscle/tendon and ligamentous, cartilage and bone structure
Locate the exact injury point; Allows the treatment to be more specific during the application of the treatment modalities
Identify the extent of tissue damage and the presence of scar tissue; Provides valuable information regarding prognosis and the application of friction soft tissue modalities to aid on scar tissue removal.
Evaluate the fracture site
Treatment protocol
The treatment care should aim to restore the shoulder alignment, the soft tissue muscles/tendon and ligamentous health as well as stimulating and remodelling the cartilage and bone growth.
Specific adjustments of key bones of the shoulder complex followed by a rehabilitation regime to strengthen the entire soft tissue support of the knee.
Fracture site must be healing prior to correcting the misalignments
Shoulder Dislocation reduction should be performed prior to any other treatment innervation
Soft tissue and cartilage healing protocol
Application of Low-level Laser and PEMF directly over the injured tissues to aid on the cellular level of healing as well as improving the microcirculation for the area.
Friction soft tissue therapy helps to reduce dysfunctional scar tissue
Specific stretches and strengthening to improve the resilient of the soft tissue support
Specific selected essential oil application to enhance healing
Dry Needling to promotes blood flow and enhance the soft tissue and cartilage healing.
Depending on the level injury and chronicity, a minimum of 6 weeks up to 12 weeks of treatment care may be necessary to resolve this condition.